- Suite 1335, 13/F.,
Central Building,
1-3 Pedder Street,
Central, Hong Kong MTR
Central Station (Exit G) - 3104 0802

-
Suite 1335, 13/F.,
Central Building,
1-3 Pedder Street,
Central, Hong Kong MTR
Central Station (Exit G) - 3104 0802
- Home
- Lower Limb Ischaemia / Diabetic Foot

Lower Limb Ischaemia / Diabetic Foot
下肢血管阻塞 / 糖尿足
Lower Limb Ischaemia
What Is PAD?
Lower limb ischaemia (often known as peripheral arterial disease or PAD) is due to the deposition of cholesterol inside the arteries causing hardening (atherosclerosis) and narrowing of the arteries resulted in restricted blood flow to the limb.
Silent PAD
- The body adapts to the narrowed arteries by opening up smaller arteries for blood to flow around (Collateral circulation). Hence, PAD may not have symptoms until the artery has narrowed by 60 percent or more. However, the life expectancy for a person with silent PAD is greatly reduced with six times higher risk of dying from heart disease. It is important to check for PAD if someone has several of the risk factors including smoking, diabetes, advanced age of over 70, history of heart disease, and hypertension.
Intermittent claudication
- Exercise induced cramping pain in the leg is called intermittent claudication and is the initial symptom of peripheral arterial disease. At rest the circulation is sufficient, but when walking the narrowed main artery taking blood to the leg cannot supply enough blood. This causes cramping pain which subside after rest. One out of 4 patients with claudication has worsening of symptoms, and 1 in 20 patients would eventually require an amputation.
Critical limb ischaemia (CLI)
- As the disease progress, aching pain occurs in the toes and feet even during periods of inactivity (rest pain). Rest pain typically wakes up the patient at night and prompts the patient to hang the leg over the bed or getting up to walk around to relieve the pain. Toe and foot sores do not heal and often deteriorate and become gangrenous. CLI is a severe stage of PAD and will not improve on its own! It needs immediate medical attention even surgical treatment to prevent amputation.
Do I have lower limb ischaemia?
Sign and symptom of lower limb ischaemia
- Exercise induced calf muscle cramping pain
- Pain at rest: ischemic rest pain is described as a burning pain in the arch or distal foot that occurs while the patient is recumbent but is relieved when the patient returns to a position in which the feet are dependent
- Lose of tissue: Non-healing wounds and gangrene
- Cold extremity
Diagnosis of PAD
- Apart from a detail medical history and clinical examination. Non-invasive tests are performed to diagnose and determine the extent of the disease. Blood pressure measured at the ankle is compared with that measured at the upper arm to give a pressure ratio i.e. ABI. ABI provides an objective measure of the lower limb circulation. Apart from diagnosing lower limb ischaemia it also predict the risk of future problems from systemic atherosclerosis.
- After ischaemia is established Duplex scan is used to localize the arterial narrowing. Invasive investigation such as CT angiogram, MR angiogram or digital subtraction arteriogram is often necessary for the planning of intervention.
ABPI to assess the overall perfusion of the lower limb
- Blood pressure cuffs are placed around the ankles and arms. These cuffs will be inflated to occlude blood flow. As the cuffs are deflated, a pencil shaped ultrasound device (called a Doppler probe) is used to detect the return of blood flow. The blood pressure at which blood flow start to return is recorded. Pressure at the ankle is divided by the pressure at the arm to establish an ankle to brachial pressure ratio or ABPI. This index provide a sensitive and specific indicator of the lower limb arterial blood supply
Ankle-brachial Index
- ABPI of less than 1.00, is associated with future risk of heart attack and/or stroke.
- An ABPI value between 0.40 – 0.80 is moderately decreased and often experience some symptoms such as pain in the legs induced by walking.
- An ABPI value of less than 0.40 indicates severe ischaemia, opinion of vascular surgeon on the benefit of invasive intervention is urgently required.
- ABPI can be performed every year to assess whether the disease is getting worse.
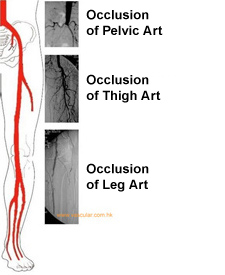
Arteriogram to localize the site of narrowing or obstruction
- ABPI of less than 1.00, is associated with future risk of heart attack and/or stroke.
- An ABPI value between 0.40 – 0.80 is moderately decreased and often experience some symptoms such as pain in the legs induced by walking.
- An ABPI value of less than 0.40 indicates severe ischaemia, opinion of vascular surgeon on the benefit of invasive intervention is urgently required.
- ABPI can be performed every year to assess whether the disease is getting worse.
Arteriogram to localize the site of narrowing or obstruction
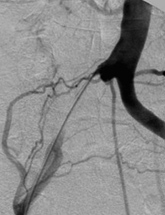
A map of the arterial tree or arteriogram (angiogram) is performed when necessary to plan for intervention
- CT Angiogram
- Digital Substraction Arteriogram
Relatively normal part of the arterial tree is punctured. A fine long tube is inserted, then contrast is injected at near the abnormal arteries. X-ray is taken to give a detail view of the abnormal vessels.
Conservative treatment
- Anti-platelet medication
- Blood pressure control
- Cessation of smoking
- Diet, to avoid overweight and have a low fat diet
- Exercise therapy
- Foot care
- Glucose control for diabetes
- HMG CoA reductase inhibitor i.e. statin should be taken
Foot Care:
When blood flow to the legs is insufficient for the healing and for the delivery of medicine to the wound, minor injuries to the feet often progress relentlessly and become serious infection or gangrene. Foot care to prevent injury is always better than regret.
- Wash feet daily: Keep clean and dry carefully especially between the toes.
- Use moisturizing cream to prevent skin crack if the skin is too dry, but avoid getting it between the toes.
- Inspect feet and toes daily: for cuts, bruises, sores, redness, swelling, and drainage.
- Wear thick, soft socks: Avoid socks with seams, which could rub to cause blisters.
- Proper fitting shoes: Shoes should be comfortable and should not require a "break-in" period. Shoes should have leather or canvas uppers, leave room for toes to wiggle freely.
- Don't wear high heels, sandals, and shoes with pointed toes: These put undue pressure on parts of the foot and contribute to foot ulcers. Open-toed shoes and sandals with straps should be avoided. Wear appropriate athletic shoes when exercising
- Never walk bare feet, even in your own home
- Don't wear anything that is too tight around the legs, this can constrict circulation
- Cut toenails straight across: Never cut into the corners, which could trigger an ingrown toenail.
-
- Never try to remove calluses by yourself: Preparations that remove corns can cause chemical burn. Never try to cut calluses as the risk of foot injury is too high.
- Avoid strong chemical, disinfectants, and extreme temperatures
- Don't use hot water bag, it can cause skin burn
Exercise therapy for patient with claudication
- Walking exercise increases the speed, distance, and duration of walking before symptoms occur. Exercise also improve the overall health. Exercise helps maintain an ideal body weight, lowers blood pressure, increases good cholesterol (HDL), reduces triglycerides, and improves the overall condition of the heart and blood vessels.
- The insufficient blood supply that causes the leg pain is also the stimulus for the ability to eventually walk longer. Exercise that do not result in claudication pain, such as bicycling, is not effective for improving claudication. Walk until near-maximum claudication pain, then rest until pain subsides. The exercise-rest-exercise cycle is repeated several times so that a total of at least 35 minutes of walking is achieved. To gain the benefit one should walk at least 3 times a week. Improvements become evident over 1-2 months. Regularity is the hallmark, as many patient with PAD also have IHD they should avoid strenuous exercise. Pain in the leg is expected, pain that occurs elsewhere in the body is an indication to stop. Pain that occurs in the chest, arms, neck, or throat could be a sign of insufficient blood flow to the heart.
What are the treatment options?
- Treatment is tailored to the severity of the disease, the earlier a diagnosis is made and treatment started the less serious the consequences. If symptoms worsen, treatment options include endovascular procedure or bypass surgery. These interventions can restore blood flow to the areas of skin breakdown. When treatment is delayed, the situation become too advanced and there may not be usable limb to save. The last recourse would be limb amputation.
Endovascular therapy
- Angioplasty with or without stent
- Stretch a short narrowing in the main trunk artery with a tiny balloon to improve blood flow.
- After angiogram is performed to have a road map of the areas of blockage the collapsed angioplasty balloon is positioned into the narrowing. The balloon is inflated to stretch it open and thus allow more blood to flow through. In special situation, a tubular metallic mesh scaffolding device, known as a stent, is fitted onto the balloon, and when the balloon is inflated and then deflated, the stent is embedded into the wall of the artery and is left in place holding the artery open. After the procedure the catheter in the groin is removed. Steady pressure is put on the groin for a few minutes and allows the hole to seal. The patient will need to lay flat for a few hours and keep the puncture site at rest.
Risk of angioplasty
Although the procedure is considered safe certain problems may develop.
- In uncommon situations, additional procedure may need to stop the bleeding in the groin.
- Ruptured or damaged artery is very unusual, yet may require emergency surgery.
- Problems with the kidney function as a result of the x-ray contrast used.
Does angioplasty work?
- The major limitation is re-narrowing of the angioplasty site. Generally, the larger the artery, the longer the artery stays open after angioplasty. Arteries below the groin, and worse yet, below the knee, tend to re-narrow faster.
Vascular reconstruction
- Bypass surgery has been used to treat patients with PAD for many decades. The likelihood of success, the durability, and the type of individuals most likely to benefit are known to the vascular surgeon. Arteriogram is performed to pinpoint the exact site of the blockages before surgery.
Endarterectomy
- The artery is opened along the blockage and the atheroma causing obstruction of the artery is peeled away. The surgeon will then close the artery with a patch of vein to make the operated artery wider and less likely to re-narrow from scarring. Endarterectomy works best for short complete blockages in the groin (femoral arteries).
Bypass surgery
- Bypass grafting is the re-routing of blood from above an obstruction to below an obstruction. It is usually reserved for longer and multiple levels of blockages along the arterial system. Bypasses have names that describe the artery above and below the blockage.
- A tube (graft or conduit) is required to carry blood. Artificial grafts are of various size and work best for large arteries that require large conduits. For bypasses down the leg, patient's own vein, preferably the saphenous vein is used as the conduit.
Risk of bypass surgery
- All bypasses have an expected patency (time while the bypass remains open and continues to function) In general, the further down the leg the shorter the patency of the bypass. The risk of death associated with bypass surgery is about one in twenty. Leg complications include wound infections and breakdown of incisions. The vast majority eventually heal. Swelling of the operated leg often gets better with time.
Diabetic Foot
- The prevalence of diabetes (DM) in Hong Kong is on the increase. More than 12% of the 7 million people of Hong Kong are older than 65-years old. About 14% of those aged over 65 have diagnosed DM. Our survey revealed that 13% of patients aged over 40 attending the diabetic clinic have evidence of lower limb ischaemia.
- Two third of patient with the most advanced ischaemia (critical limb ischaemia) have underlying diabetes. Diabetic patient often have arterial obstruction at the leg level. Fortunately, foot arteries are almost invariably remain open, which allows for distal arterial reconstruction. Our experience in Hong Kong concurred with most published data that arterial reconstruction is almost always possible and usually successful in patients with diabetes. Distal arterial reconstruction to the foot level has been demonstrated to be a technically feasible and highly effective treatment to save the leg of diabetic patient with infected ulcer or gangrene.
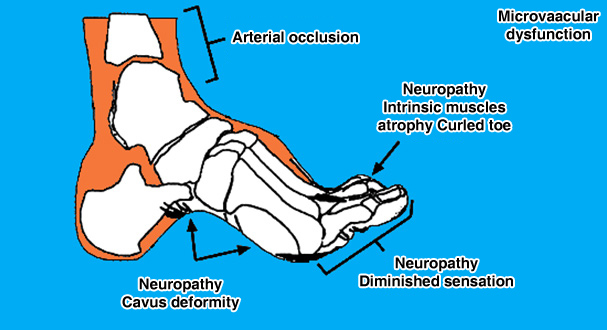
Cause of diabetic foot ulcer
- Diabetes patients have compromised defense to infection and the long-term effects of diabetes are damage to the eyes (retinopathy), nerves (neuropathy) and arteries (arteriopathy)
- The nerve problems cause foot deformity and decreased sensation. These predispose to foot injury
- In the event of co-existing poor blood supply the injury cannot heal
- In diabetic patient the ulcer quickly become infected and lead to spreading infection and gangrene
- In addition, diabetic patients often have poor vision (retinopathy) which deprived them the ability to detect foot problems at an early stage.
- Diabetic foot lesion
- Gangrene
- Ulcer
- Non-healing amputation wound
How to avoid limb amputation?
- The key to prevent amputation in diabetic patients is regular foot screenings for the detection of at risk foot and early recognition of foot lesion. Diabetic patients with foot ulcer should have the blood supply evaluated as soon as possible. Spreading foot infection in diabetic patient with insufficient blood supply is a medical emergency. Do not delay for conservative treatment, early surgical intervention is often the only opportunity to save the limb and life.
- Diabetes are more likely than other patients to have distal disease and are less amenable to angioplasty. Compared with amputation, revascularization is more cost-effective and is associated with better perioperative morbidity and mortality. Limb preservation should be the goal
- Bypasses to foot artery
- The key to prevent amputation in diabetic patients is regular foot screenings for the detection of at risk foot and early recognition of foot lesion. Diabetic patients with foot ulcer should have the blood supply evaluated as soon as possible. Spreading foot infection in diabetic patient with insufficient blood supply is a medical emergency. Do not delay for conservative treatment, early surgical intervention is often the only opportunity to save the limb and life.